This article focuses on the first prize of the Shanghai Municipal Science and Technology Progress Award for 2022, awarded for the research and application of "Key Technologies for the Clinical Diagnosis and Treatment of Chronic Pancreatitis." The award was received by a team led by Professor Liao Zhuanzhuan, the director of the First Affiliated Hospital of Naval Medical University (Shanghai Changhai Hospital).

A global challenging illness – chronic pancreatitis
In the human body, the "pancreas" is a rather inconspicuous organ, weighing about 200 grams, yet it is one of the most crucial organs of the body. It is associated with both the notoriously deadly pancreatic cancer and the high-mortality “acute pancreatitis.” However, few people are aware of the existence of “chronic pancreatitis.” Years ago, this excruciating disease was considered incurable; patients had no choice but to rely on painkillers for relief, eventually developing an addiction to them and suffering from severe physical decline. There is also a risk of cancer development associated with this condition. At that time, chronic pancreatitis was recognized globally as a significant challenge to treat.
After over 20 years of effort, Professor Liao Zhuanzhuan’s team at the First Affiliated Hospital of Naval Medical University (Shanghai Changhai Hospital) conquered this world-class challenge by using shockwave therapy to break up stones in the pancreas. This innovative approach worked effectively to produce excellent treatment outcomes and gained wide praise from patients. Shanghai has since evolved from a national center for chronic pancreatitis treatment to a global center for the same. The project titled "Research and Application of Key Technologies for the Clinical Diagnosis and Treatment of Chronic Pancreatitis" won the first prize of the Shanghai Municipal Science and Technology Progress Award in 2022.
Living in agony with no way out—an enduring medical challenge worldwide
The food we consume passes through the mouth, throat, esophagus, stomach, small intestine, and large intestine in sequence. The small intestine is further divided into the duodenum, jejunum, and ileum. The duodenum, measuring about 20–25 centimeters, is particularly significant, as it receives the pancreatic duct and bile duct that lead to the small intestine. The digestive juices secreted by these two organs flow into the small intestine, aiding in food digestion, nutrient absorption, and providing energy for the body’s survival.
The primary function of the pancreas is to secrete digestive enzymes, serving both exocrine and endocrine roles. The endocrine part secretes insulin, which plays a vital role in regulating blood sugar levels. The exocrine gland consists of acini and ducts, primarily secreting lipase, protease, and amylase among other pancreatic enzymes. Although this may appear straightforward, the inner workings of the exocrine glands involve highly precise assembly lines. "The acini secrete digestive enzymes, which remain inactive and in a dormant state while being transported through the pancreatic ducts. Upon entering the duodenum in the small intestine, the intestinal juices activate these enzymes via intestinal kinases, breaking down food for absorption," Professor Liao explains. This process can be likened to the “transport of hazardous materials,” where the pancreatic duct acts like a river, the pancreatic acini are akin to a "chemical factory" upstream, and the small intestine serves as the final "assembly plant," where the inactive enzymes are reactivated and perform their functions after arriving in the small intestine. However, if any errors occur during this process, disease can arise.

The pancreas is a vital organ with both exocrine and endocrine functions.
“Acute pancreatitis is usually linked to excessive alcohol consumption or gallstones, which cause bile to flow into the pancreatic duct. This process activates inactive digestive enzymes in the duct, initiating a dangerous phase of ‘auto-digestion,’ producing amino acids, and further activating more pancreatic enzymes, leading to a chain reaction. When the various digestive substances cannot be expelled from the pancreas and enter the bloodstream, they trigger an inflammatory response that severely damages multiple organs, resulting in multi-organ failure. This is the underlying mechanism of the highly fatal severe acute pancreatitis. The reason the stomach and small intestine do not experience such an alarming ‘auto-digestion’ is that they possess a mucosal barrier, primarily composed of bicarbonate and mucus. The pancreatic duct, however, lacks this protective substance,” explains Professor Liao. If acute pancreatitis can be described as a “raging fire,” chronic pancreatitis can be characterized as a “gentle simmer.”
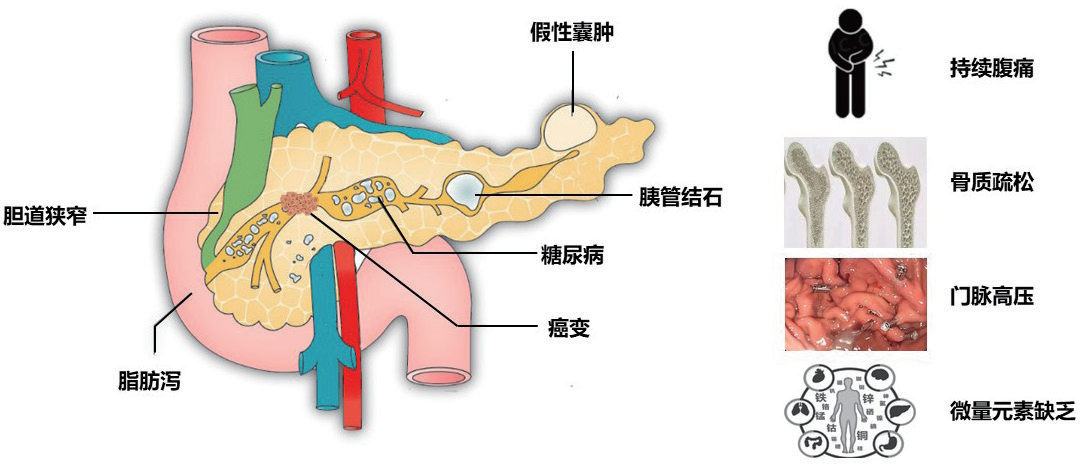
The most prominent feature of chronic pancreatitis is the recurrent inflammation resulting in fibrotic changes inside the pancreatic duct. This fibrosis acts as a form of self-protection for the organ because the pancreas occupies a uniquely vulnerable position, located retroperitoneally, adjacent to major blood vessels and organs in a confined space. Once stimulated, it can cause intense pain, leading patients to experience severe abdominal pain for years, at times even every few months. When a part of the body is injured, it develops a scab; a similar principle applies to the internal fibrotic changes of organs—repeated fibrosis leads to an increasingly larger fibrous shell. The digestive enzymes produced by the pancreas contain calcium ions, while the epithelial cells of the pancreatic duct secrete water and bicarbonate ions, originally meant to facilitate “transport” and maintain an alkaline environment within the duct. However, under the stimulus of this unique inflammatory response, a reaction occurs between these two components, forming calcium carbonate, which is the main constituent of pancreatic stones. After stones form, the pancreatic duct expands, pancreatic enzyme secretion increases, leading to a continuous deterioration of the condition.
About 10% of chronic pancreatitis patients experience pancreatic atrophy, resulting in insufficient enzyme secretion, which can be treated with external replacement therapy, restoring digestive and carbohydrate metabolism functions with lifelong medication. The remaining 90% of patients, however, present with pancreatic stones.
“The pancreatic ducts are quite narrow, with an average diameter of around 3 to 4 millimeters in adults. Endoscopic procedures cannot effectively access them for minimally invasive surgery. Historically, surgery was the only option for pancreatic issues, but pancreatic surgery is recognized as one of the most difficult surgical procedures globally, often resulting in significant complications. Generally, only early-stage pancreatic cancer patients undergo surgery to save their lives. Additionally, after surgery for pancreatic stones, recurrence of stones can occur due to the trauma inflicted. Patients continue to endure immense suffering but are left with pain medications for relief,” states Professor Liao.
Innovative application of shockwaves to achieve satisfactory healing results
Overcoming the treatment challenges of chronic pancreatitis began 21 years ago when Chinese Academy of Engineering Academician Li Zhaoshen identified it as a research direction for his protégé, Liao Zhuanzhuan, who was then a master's student under Li.
At that time, a “shockwave” technology was being tested in the treatment of kidney stones via “extracorporeal shockwave lithotripsy.” Shockwaves possess a unique characteristic: they can traverse identical density environments without impact but cause disruption when encountering environments of differing densities. In early medical experiments using shockwaves to treat kidney stones, physicians would have patients sit in a tub fitted with a shockwave emitter. Since the density of kidney stones is significantly higher than that of the human body, shockwaves effectively break the stones during treatment.
Professor Liao and his colleagues began to consider whether this shockwave technology used for kidney stones could also be adapted for treating chronic pancreatitis. The idea was promising, yet the journey was fraught with challenges.
“We brought some patients to a medical facility specializing in kidney stone treatment, but we experienced repeated failures. Unlike other stones, pancreatic stones adhere tightly to the walls of the duct, akin to having ‘teeth’ on the pancreatic duct, making them particularly stubborn and difficult to detach. Upon applying shockwaves to the stones, the resulting shock would cause vibrations within the pancreas itself. Given that numerous nerves surround the pancreas, this leads to excruciating pain, causing patients to instinctively recoil, preventing targeted treatment,” the professor recounted. The team then sought solutions to tackle these various obstacles one by one.
Utilizing X-ray imaging for precise stone localization and employing anesthesia, they enabled patients to undergo lithotripsy from the front of the body while under general anesthesia, additionally administering sedatives to enhance treatment efficacy. Many of the stones would drop directly into the small intestine, where they were decomposed by digestive fluids, allowing for immediate clearance of painful symptoms.
However, some shattered pancreatic stones would scatter in the duct and obstruct the flow of pancreatic enzymes, potentially triggering inflammation again—this was the most significant complication in the “remote control” therapy. To counteract this, the team prepared anti-inflammatory suppositories (indomethacin) for patients as a preventative measure. Furthermore, to enhance the effectiveness of the “remote control” technique, the team developed specific technical protocols and guidelines, detailing the frequency, energy levels, and usage methods of shockwaves, ensuring the scientific and standardized nature of the treatment. Thus, a world-class major problem was comprehensively overcome!
Minimally invasive treatment for pancreatic duct stones in chronic pancreatitis
Today, the treatment of chronic pancreatic stones has evolved into a unique specialty of Shanghai Changhai Hospital, attracting patients from across the nation and around the globe. Currently, Professor Liao’s research team has conducted approximately 10,000 treatment sessions with a success rate nearing 100%. Hospitals both internationally and domestically are seeking to learn from their practices. Chronic pancreatitis patients no longer need to endure agony; treatment costs around 20,000 yuan and typically allows patients to recover and be discharged within a week. Follow-up studies indicate that the recurrence rate of chronic pancreatitis treated through this method is also remarkably low.

Minimally invasive treatment for pancreatic duct stones in chronic pancreatitis
The onset of chronic pancreatitis is also associated with genetic mutations in the human body. Some cases are linked to chronic alcohol abuse and overeating, leading to excess bile secretion that irritates the pancreas. However, there are other patients with commendable lifestyle habits who still develop this ailment. Professor Liao's team has conducted in-depth research into the biological basis of chronic pancreatitis and discovered that it is indeed associated with genetic mutations. "Certain gene mutations lead to an overproduction of pancreatic proenzymes, while others, which function like ‘police officers’ to regulate and inhibit excessive production, lose their functionality due to mutations. We’ve identified over 10 involved genes, and we are currently working on restoring the ‘SPINK1’ gene mutation unique to the most common chronic pancreatitis types among the Chinese population, aiming to alleviate patients’ suffering from its root cause,” he explains.
Developing “capsule robots” for unprecedented diagnostics and treatment within the life river
If we consider the human digestive tract as a river of life, the pancreas is a significant tributary. However, Professor Liao’s research team does not limit their vision solely to this tributary; they aspire to explore the entire “river of life,” which was the second research challenge set forth by Academician Li Zhaoshen: to break through the technical limitations of endoscopic procedures.
Despite the presence of gastroscopy and colonoscopy techniques more than 20 years ago, a segment of the digestive tract remains a human “blind zone,” an inaccessible “black box.” Neither gastroscopy nor imaging CT can visualize it, specifically the extended 5-7 meter small intestine, where ailments such as Crohn's disease manifest ulcers on the internal wall.

Professor Liao Zhuanzhuan performing extracorporeal shockwave lithotripsy for chronic pancreatitis.
The objective of Professor Liao's team in developing the first-generation capsule robot was to “visualize” the conditions inside the small intestine.
Subsequently, the team embraced a more ambitious goal: to create a capsule endoscope that could “walk with legs” throughout the entire digestive tract, under the control of medical personnel. Based on magnetic principles, the team developed the second-generation capsule robot—the magnetic-controlled capsule robot—allowing patients to lie beneath a magnetic detection device. A tiny capsule robot, about the size of a fingernail, travels through the esophagus into the patient’s body, functioning like a “remote sensing satellite,” where doctors can adjust its movement and view the condition of every nook and cranny within the stomach and intestines. This technology allows for inspections of esophageal varices and assessments of the damage to the esophagus caused by taking aspirin, as well as early screenings for gastrointestinal tumors.