With at least hundreds of millions of people worldwide infected with the new coronavirus (SARS-CoV-2), the ensuing "long Covid" (long-term impact of new coronary pneumonia) has become another pandemic. Fatigue, difficulty concentrating, and loss of taste and smell are common symptoms of COVID-19.
The latest research from the University Medical Center Rotterdam in the Netherlands shows that these symptoms in patients with COVID-19 are related to the level of inflammation in the nerves of the brain. The research team tracked important brain inflammatory markers and demonstrated severe neuroinflammation in patients with COVID-19 through imaging methods. The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.
The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.
Previously, autopsy histopathology studies have shown extensive inflammatory responses in organs, including the brain, of acute COVID-19 patients. Microglial activation is the most common pathology found in brain autopsies of COVID-19 patients, with the highest levels of diffuse microglial activation in the olfactory bulb, medulla oblongata, brain stem, and cerebellum. However, to date, there have been no in vivo studies of neuroinflammation in COVID-19 patients or after recovery. Research from the University of Rotterdam in the Netherlands fills that gap.
The study focused on microglia because these are phagocytic cells that colonize the brain and are antigenically enhanced, morphologically stretched, and functionally active in response to inflammatory stimuli. When inflammation occurs, microglia can rapidly proliferate, increase or re-express MHC antigens, migrate and change into a phagocyte-like form (amoeba-like) and burst to secrete a large number of cytokines and cytotoxic substances.
Microglia are distributed in all parts of the brain and are 5 times more abundant in gray matter than in white matter. There were more microglia in the hippocampus, olfactory lobe, and basal ganglia than in the thalamus and hypothalamus, but the least in the brainstem and cerebellum. Microglia are widely considered to be the main immune effectors within the central nervous system and are involved in human neurological disorders such as HIV encephalopathy, Parkinson's disease, Alzheimer's disease (senile dementia), and multiple sclerosis.
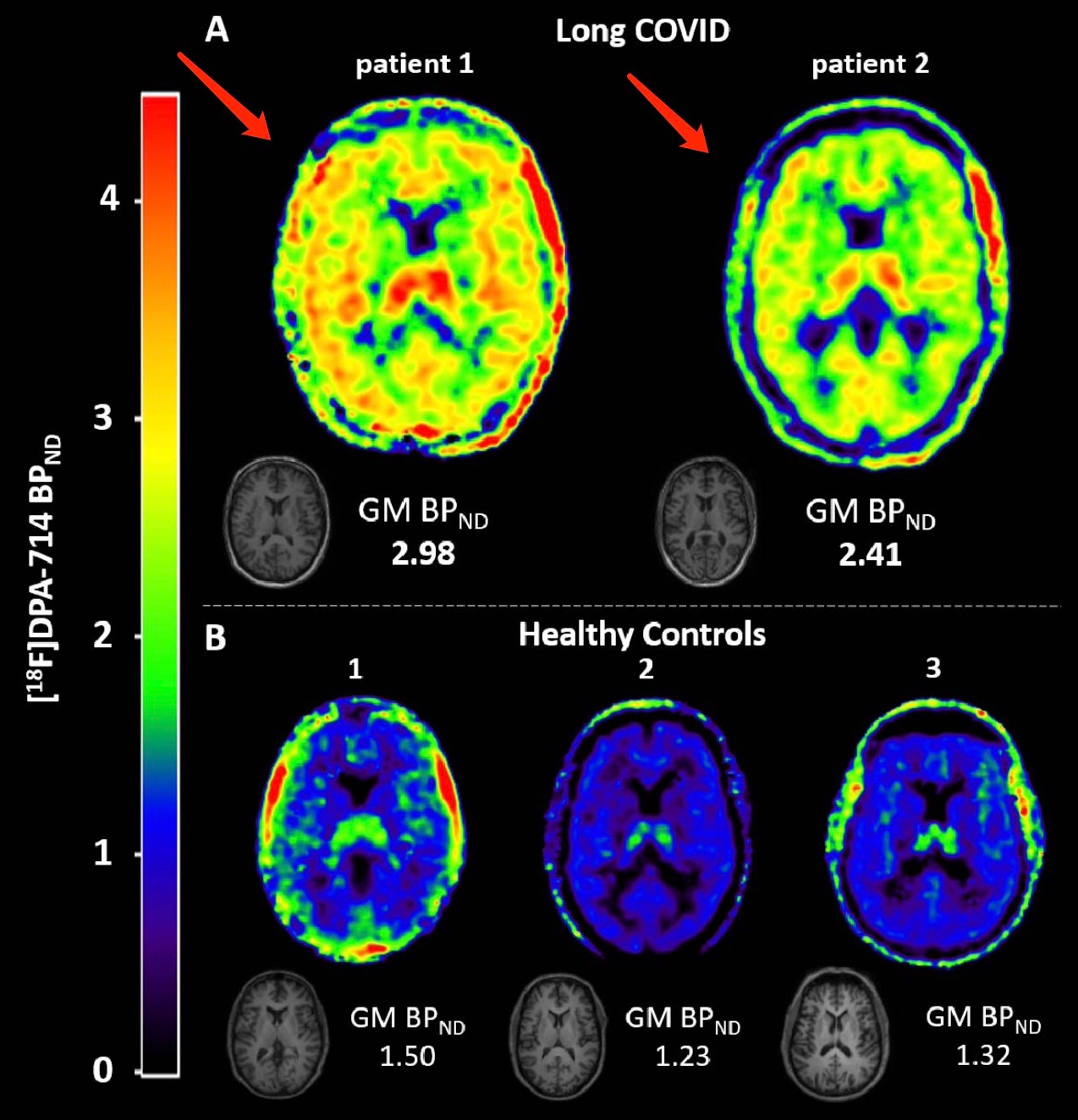
The study used positron emission tomography (PET) to observe [18F]DPA-714 levels in the brains of patients with long-term new crowns, thereby assessing the activation of inflammation by microglia in the brain nerves of patients. [18F]DPA-714 is a PET tracer, a high-affinity transporter protein (TSPO, a mitochondrial outer membrane protein expressed in activated microglia and macrophages in the brain as a marker of neuroinflammation substance) ligand. [18F]DPA-714 can be used to evaluate inflammation-specific imaging in various neuroinflammation models and brain tumor models.
The first COVID-19 patient in the University of Rotterdam study in the Netherlands was a Dutch woman in her 50s who was healthy, working full-time and living a fulfilling life before infection. She tested positive for nucleic acid in December 2020, and during the acute phase of the infection, she was not hospitalized and did not require treatment. Since the infection, she has developed severe fatigue, difficulty concentrating, anosmia and anosmia, headaches and some vision problems. Her symptoms prevented her from working, and her symptoms persisted to this day, 15 months after infection.
The second COVID-19 patient in the study was a Dutch man in his 60s who was healthy and working full-time before contracting SARS-CoV-2. He tested positive for nucleic acid in March 2020. During the acute phase of SARS-CoV-2 infection, he was hospitalized in the nursing unit for 15 days. After 10 days, he was admitted to the intensive care unit (ICU) for a day with breathing problems. During his hospital stay, he received standard medical treatment. Since the infection, he has suffered from severe fatigue and difficulty concentrating, and has been unable to work. Although things have since improved, his symptoms have persisted to this day, 24 months after infection.
The researchers performed dynamic 60-minute [18F] DPA-714 PET scans of arterial blood samples in 2 patients with long-term new crowns. To assess tracer metabolism, the researchers compared the [18F]DPA-714 metabolite in the blood of two COVID-19 patients with the metabolites in the blood of all other available subjects. They assessed activity concentrations in whole blood, corrected for injected activity and tracer maternal fraction from arterial blood samples.
The study found that [18F]DPA-714 binding in all brain regions was severely elevated in patients with COVID-19. Whole-brain gray matter quantitative BPND (=k3/k4) obtained from its 2T4k_VB model increased by an average of 121% relative to healthy control subjects. [18F]DPA-714 binding was also elevated in COVID-19 patient 2, with an average increase of 79% in whole-brain gray matter BPND (=k3/k4) obtained from the 2T4k_VB model relative to healthy control subjects.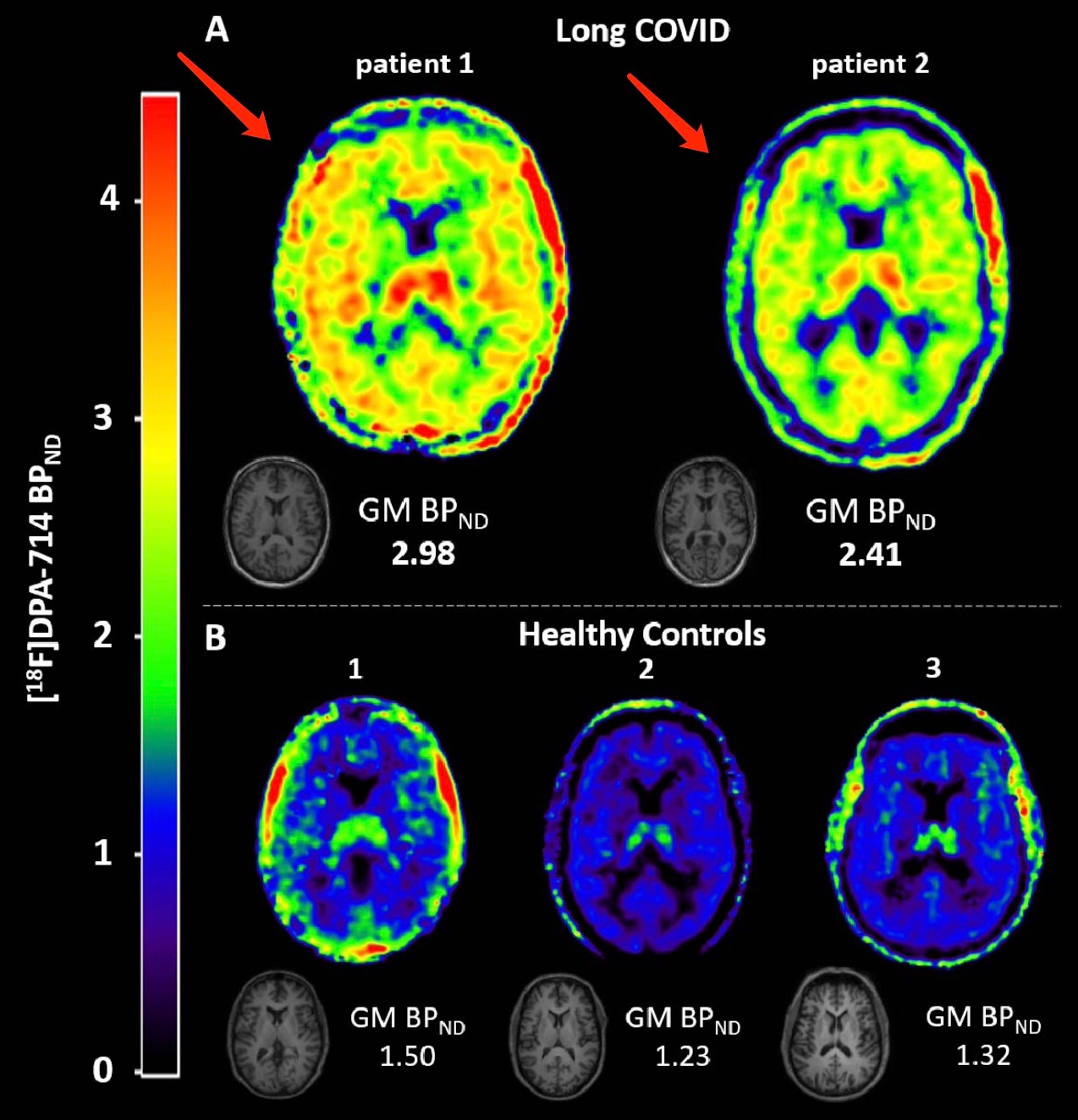 The researchers also administered a neuropsychological questionnaire to 2 subjects. Patient 1 had verbal memory deficits, mild impairment of sustained attention, severe fatigue and attention problems, and severe functional impairment. Patient 2 had visual constructive deficits, persistent attention fluctuations, fatigue, severe attention problems, and severe functional impairment.
The researchers also administered a neuropsychological questionnaire to 2 subjects. Patient 1 had verbal memory deficits, mild impairment of sustained attention, severe fatigue and attention problems, and severe functional impairment. Patient 2 had visual constructive deficits, persistent attention fluctuations, fatigue, severe attention problems, and severe functional impairment.
This research from the University of Rotterdam in the Netherlands has added an important link to the mechanism of neurological diseases in patients with chronic new crowns. Previous studies were mostly phenomenological studies. For example, in September 2021, a study by the top international medical journal BMJ (British Medical Journal) showed that in 148 intensive care unit inpatients and follow-up, 73% of the The patient suffers from delirium. The above research was jointly completed by the University of Michigan School of Medicine, New York School of Medicine and other teams. People with delirium tend to be more severely ill, have more complications such as high blood pressure and diabetes, and also appear to have more severe COVID-19-related illness, said the study's corresponding author, Phillip Vlisides, MD, of the Department of Anesthesiology at the University of Michigan School of Medicine. .
Delirium is a severe mental state disorder in which patients are often confused, agitated, and unable to think clearly. Notably, major neurological complications such as encephalopathy, stroke, epilepsy, and ataxia have been observed since the COVID-19 pandemic.
As early as April 2020, The Paper (www.thepaper.cn) reported that a research team from Tongji Medical College of Huazhong University of Science and Technology and St. Joseph's Hospital in the United States published the first online publication in the top journal "JAMA" (JAMA). Articles detailing the effects of the new coronavirus on the nervous system. Neurological symptoms occurred in more than one-third (36.4%) of the 214 patients in the study at the time.
The latest research from the University Medical Center Rotterdam in the Netherlands shows that these symptoms in patients with COVID-19 are related to the level of inflammation in the nerves of the brain. The research team tracked important brain inflammatory markers and demonstrated severe neuroinflammation in patients with COVID-19 through imaging methods.
 The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.
The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.Previously, autopsy histopathology studies have shown extensive inflammatory responses in organs, including the brain, of acute COVID-19 patients. Microglial activation is the most common pathology found in brain autopsies of COVID-19 patients, with the highest levels of diffuse microglial activation in the olfactory bulb, medulla oblongata, brain stem, and cerebellum. However, to date, there have been no in vivo studies of neuroinflammation in COVID-19 patients or after recovery. Research from the University of Rotterdam in the Netherlands fills that gap.
The study focused on microglia because these are phagocytic cells that colonize the brain and are antigenically enhanced, morphologically stretched, and functionally active in response to inflammatory stimuli. When inflammation occurs, microglia can rapidly proliferate, increase or re-express MHC antigens, migrate and change into a phagocyte-like form (amoeba-like) and burst to secrete a large number of cytokines and cytotoxic substances.
Microglia are distributed in all parts of the brain and are 5 times more abundant in gray matter than in white matter. There were more microglia in the hippocampus, olfactory lobe, and basal ganglia than in the thalamus and hypothalamus, but the least in the brainstem and cerebellum. Microglia are widely considered to be the main immune effectors within the central nervous system and are involved in human neurological disorders such as HIV encephalopathy, Parkinson's disease, Alzheimer's disease (senile dementia), and multiple sclerosis.
The study used positron emission tomography (PET) to observe [18F]DPA-714 levels in the brains of patients with long-term new crowns, thereby assessing the activation of inflammation by microglia in the brain nerves of patients. [18F]DPA-714 is a PET tracer, a high-affinity transporter protein (TSPO, a mitochondrial outer membrane protein expressed in activated microglia and macrophages in the brain as a marker of neuroinflammation substance) ligand. [18F]DPA-714 can be used to evaluate inflammation-specific imaging in various neuroinflammation models and brain tumor models.
The first COVID-19 patient in the University of Rotterdam study in the Netherlands was a Dutch woman in her 50s who was healthy, working full-time and living a fulfilling life before infection. She tested positive for nucleic acid in December 2020, and during the acute phase of the infection, she was not hospitalized and did not require treatment. Since the infection, she has developed severe fatigue, difficulty concentrating, anosmia and anosmia, headaches and some vision problems. Her symptoms prevented her from working, and her symptoms persisted to this day, 15 months after infection.
The second COVID-19 patient in the study was a Dutch man in his 60s who was healthy and working full-time before contracting SARS-CoV-2. He tested positive for nucleic acid in March 2020. During the acute phase of SARS-CoV-2 infection, he was hospitalized in the nursing unit for 15 days. After 10 days, he was admitted to the intensive care unit (ICU) for a day with breathing problems. During his hospital stay, he received standard medical treatment. Since the infection, he has suffered from severe fatigue and difficulty concentrating, and has been unable to work. Although things have since improved, his symptoms have persisted to this day, 24 months after infection.
The researchers performed dynamic 60-minute [18F] DPA-714 PET scans of arterial blood samples in 2 patients with long-term new crowns. To assess tracer metabolism, the researchers compared the [18F]DPA-714 metabolite in the blood of two COVID-19 patients with the metabolites in the blood of all other available subjects. They assessed activity concentrations in whole blood, corrected for injected activity and tracer maternal fraction from arterial blood samples.
The study found that [18F]DPA-714 binding in all brain regions was severely elevated in patients with COVID-19. Whole-brain gray matter quantitative BPND (=k3/k4) obtained from its 2T4k_VB model increased by an average of 121% relative to healthy control subjects. [18F]DPA-714 binding was also elevated in COVID-19 patient 2, with an average increase of 79% in whole-brain gray matter BPND (=k3/k4) obtained from the 2T4k_VB model relative to healthy control subjects.
 The researchers also administered a neuropsychological questionnaire to 2 subjects. Patient 1 had verbal memory deficits, mild impairment of sustained attention, severe fatigue and attention problems, and severe functional impairment. Patient 2 had visual constructive deficits, persistent attention fluctuations, fatigue, severe attention problems, and severe functional impairment.
The researchers also administered a neuropsychological questionnaire to 2 subjects. Patient 1 had verbal memory deficits, mild impairment of sustained attention, severe fatigue and attention problems, and severe functional impairment. Patient 2 had visual constructive deficits, persistent attention fluctuations, fatigue, severe attention problems, and severe functional impairment.This research from the University of Rotterdam in the Netherlands has added an important link to the mechanism of neurological diseases in patients with chronic new crowns. Previous studies were mostly phenomenological studies. For example, in September 2021, a study by the top international medical journal BMJ (British Medical Journal) showed that in 148 intensive care unit inpatients and follow-up, 73% of the The patient suffers from delirium. The above research was jointly completed by the University of Michigan School of Medicine, New York School of Medicine and other teams. People with delirium tend to be more severely ill, have more complications such as high blood pressure and diabetes, and also appear to have more severe COVID-19-related illness, said the study's corresponding author, Phillip Vlisides, MD, of the Department of Anesthesiology at the University of Michigan School of Medicine. .
Delirium is a severe mental state disorder in which patients are often confused, agitated, and unable to think clearly. Notably, major neurological complications such as encephalopathy, stroke, epilepsy, and ataxia have been observed since the COVID-19 pandemic.
As early as April 2020, The Paper (www.thepaper.cn) reported that a research team from Tongji Medical College of Huazhong University of Science and Technology and St. Joseph's Hospital in the United States published the first online publication in the top journal "JAMA" (JAMA). Articles detailing the effects of the new coronavirus on the nervous system. Neurological symptoms occurred in more than one-third (36.4%) of the 214 patients in the study at the time.



Comments